Published On: January 2017 in Kaiser Health News. Read the story here. This KHN story also ran on PBS NewsHour.
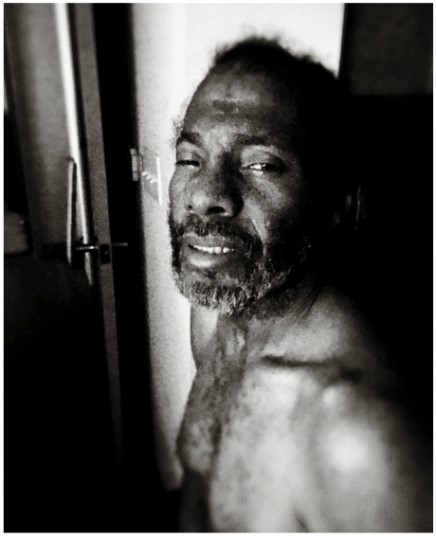
HOUSTON — Donning a protective gown, rubber gloves and a face mask, Dayna Gurley looks like she's heading into surgery. But Gurley is a medical social worker charged with figuring out why her client, a man who uses more health care services than almost anyone else in Houston, has been in three different hospitals in the last month.
The patient, who asked not to be identified, has chronic massive ulcers, AIDS and auditory hallucinations. He rents a cot in another person's home but is more often homeless, with no family to help him.