The Need
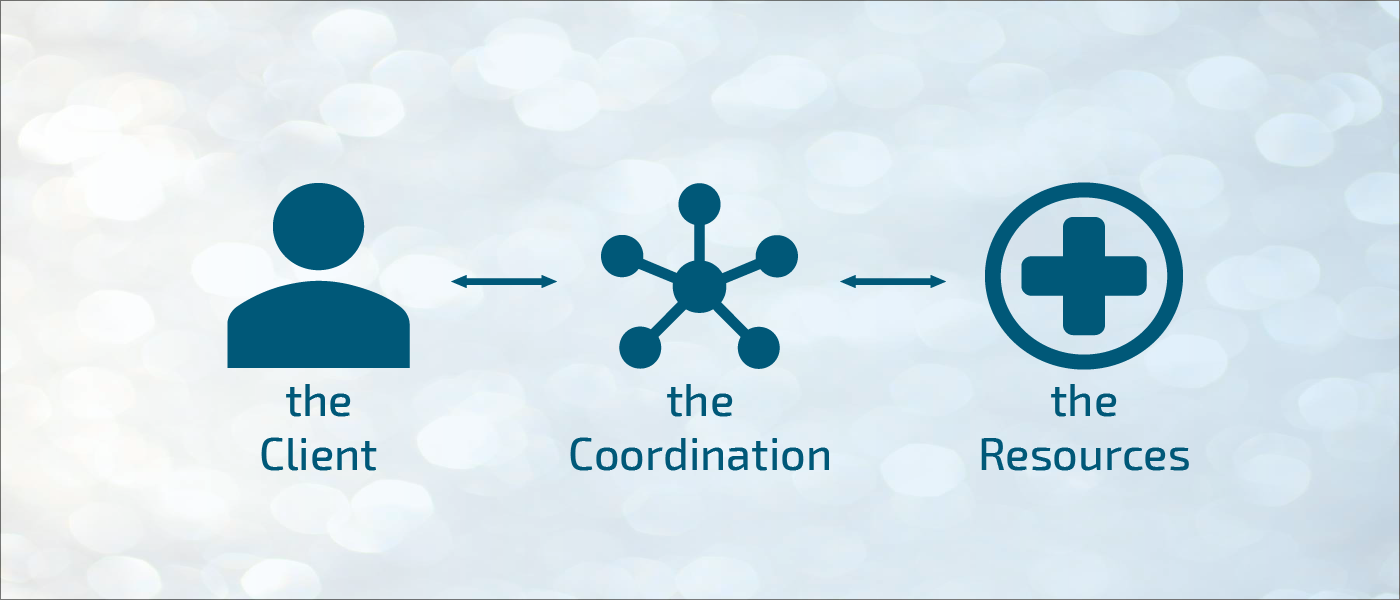
The current model of care for vulnerable populations is siloed across and within medical and social providers. Individuals who seek care from multiple agencies likely have a case manager to represent them at each provider, but these case managers lack the technology to collaboratively coordinate care across systems. As such, referrals between systems are passive, placing the responsibility of coordinating visits upon the most at-risk individuals.
50% of healthcare spending in the U.S. is consumed by just 5% of the population?
In order to get better, this 5% of high-cost patients often need social and behavioral supports that fall outside of the traditional medical domain.
To solve these issues, we have developed the Unified Care Continuum Platform, which bolsters population health at many levels to ensure accountability and coordination across provider systems.
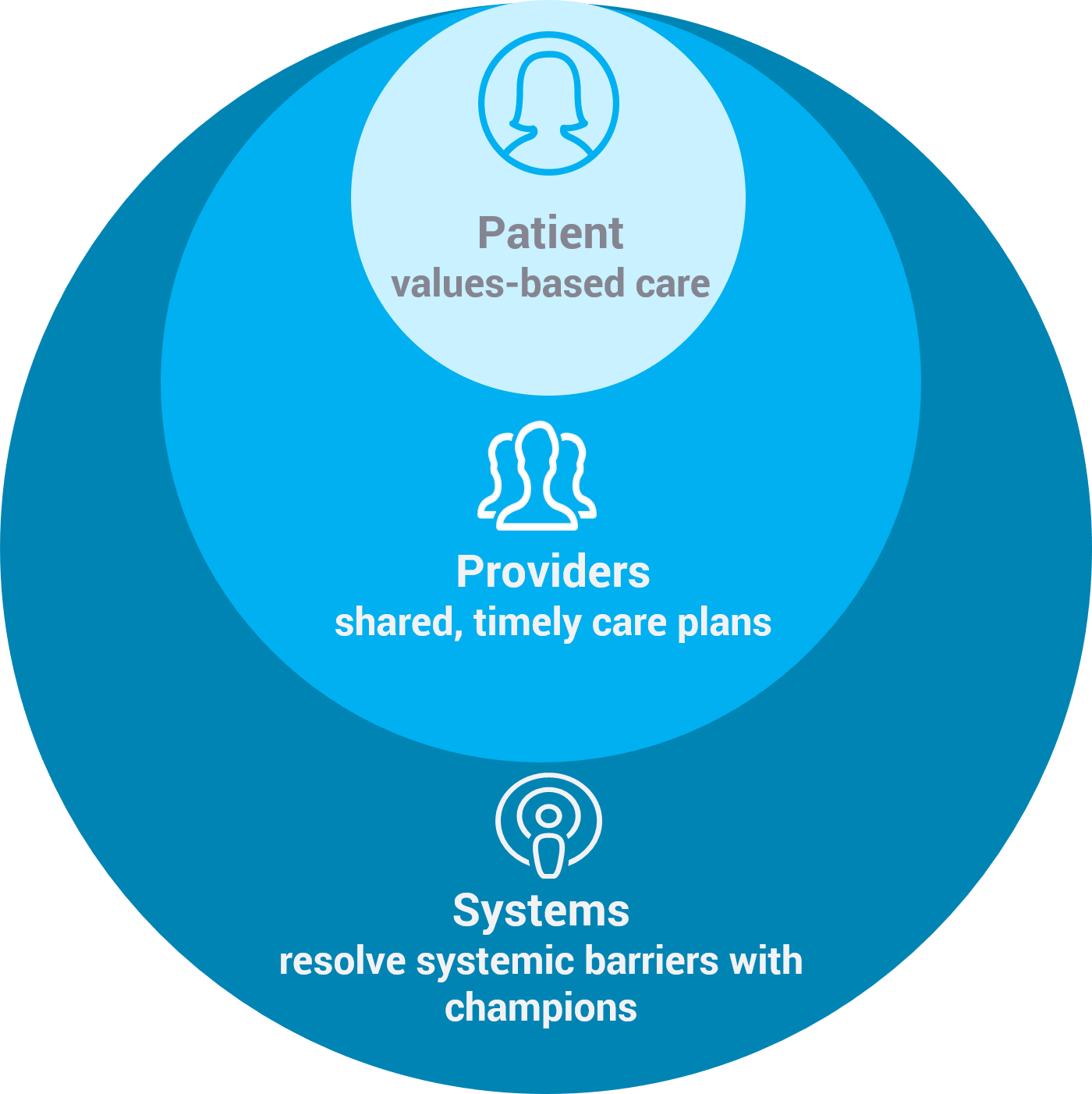
By following the evidence that 80% of an individual’s health is determined by social, economic and environmental factors, while 20% of an individual’s health is determined by clinical factors, our platform is designed to track, measure, and address these complex determinants of health – including medical, housing and transportation, income and employment status, hunger and access to nutritious foods, literacy and language, behavioral health, social integration, and much more – by linking data from disparate medical and social provider systems to create a comprehensive record for each client.
We turn the current problem-centered model of care on its head by facilitating personalized care plans that are driven by clients’ values, goals, and strengths.
Platform Overview
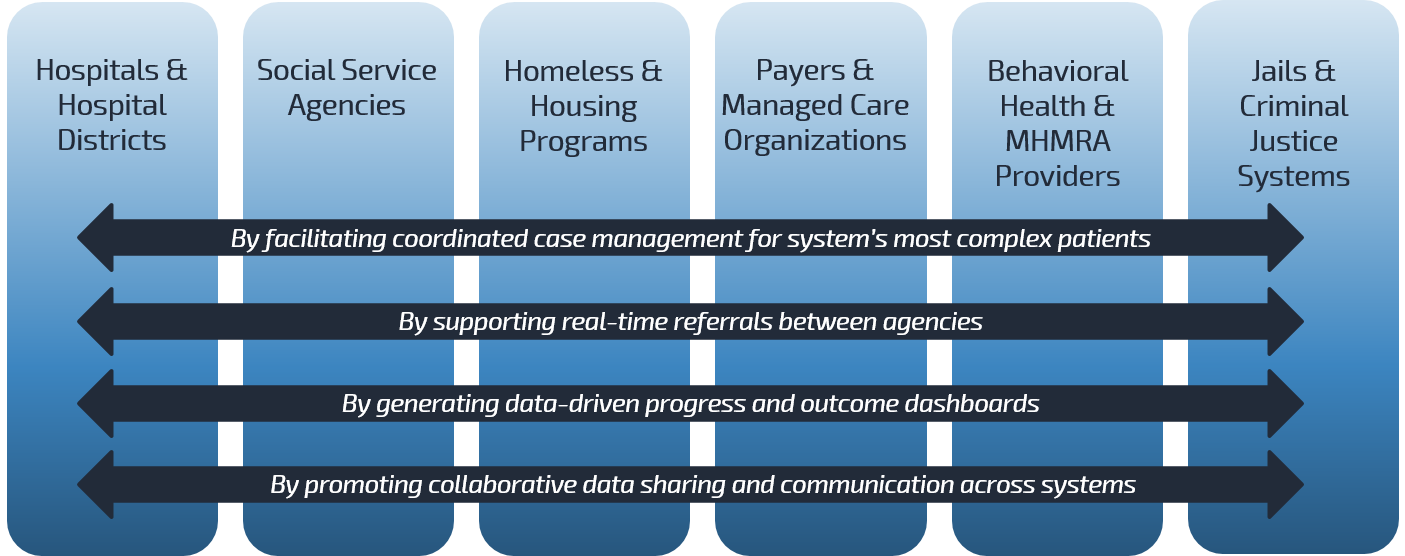
We are building a bridge between service providers to facilitate data sharing and cross-agency care coordination for Houston’s most vulnerable individuals. Through robust, cross-agency data analytics and patient care plans that are shared across agencies, our platform strengthens our region’s health safety net by empowering medical and social agencies to collaboratively address social and economic determinants of health.
The Unified Care Continuum Platform’s core functionalities include facilitating care coordination for patients with complex needs, linking need to resources in real-time, streamlining collaboration between medical and social service providers, and generating data to support advocacy for systems-level change.
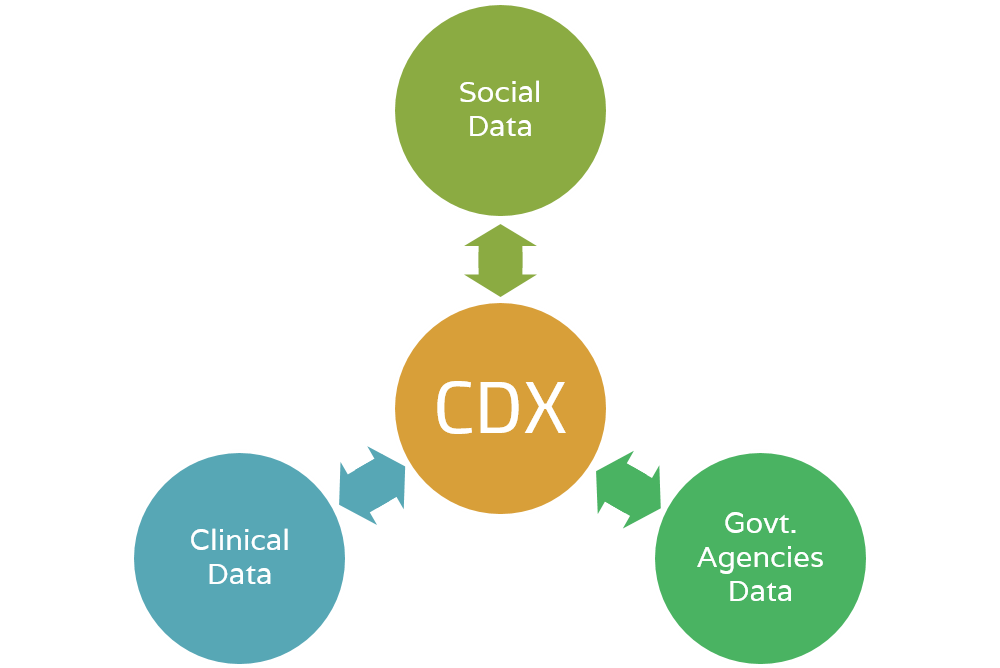
Community Data eXchange - Merges social and medical records
The Community Data eXchange is a data platform that merges patient data from medical and social service agencies.
By linking data from over 25M+ client visits to various systems (i.e. hospitals, EMS calls, homeless shelters, insurance companies, recovery/rehabilitation centers, and more), the Community Data eXchange bridges the communication gap between siloed systems and helps us see a more complete view of utilization and needs.
By using service utilization as an indicator of patient complexity, the Community Data eXchange helps healthcare providers and payers, social service agencies, and local governments understand population health needs and service gaps within a community.
One way we use the Community Data eXchange is to identify the small number of individuals in a given population who rely on the greatest number of services. Using this measure a proxy for social and medical vulnerability, the Community Data eXchange informs the selection process for patients who stand to benefit the most from personalized care coordination, driven by patients’ values and goals.
-
The Community Data eXchange enables medical and social agencies to collaboratively recognize clients they have in common, identify common service gaps in the community, and work together to overcome systemic barriers to health.
Because we understand health to be the complex interplay between social, behavioral, and medical factors, we must expand our definition of healthcare to include an integrated response across social, behavioral and medical domains.
By linking patient records across social and medical agencies, the Community Data eXchange allows providers to see the specific social vulnerabilities of their patients alongside their pathologies.
Since many medical conditions are exacerbated and even caused by social vulnerabilities, providers that understand their patients' complex needs are better equipped to engage with patients and develop effective care plans.
-
Agencies that provide social services to vulnerable individuals can partner with PCIC to discover how their client population utilizes other community services. This helps team deliver meaningful patient segmentation that considers social and medical risk factors for health.
Our data discovery helps social agencies understand how participation in their programs reduces the frequency and cost of participants’ emergency services, homeless shelter check-ins, jail bookings, and more.
-
On an individual level, the most socially and medically complex patients will be met with personalized care coordination to holistically address their health needs.
-
Our long-range strategy includes understanding widespread data on social and medical service utilization, a proxy for unmet need and disparity, as a means of informing policymakers of our community’s most pressing and unmet needs. Once the system can recognize, measure, and respond to the factors that affect population health, policies and procedures can be enacted to help overcome these systemic barriers to health.
Community Resource eXchange - Connects the right resource to the right person
The Community Resource eXchange exists to facilitate effective resource referrals between siloed medical and social agencies.
Developed in a collaborative API-based model, the Community Resource eXchange links existing resource databases (such as Welnity, with the architectural support to enable linking to sources such as 211, Aunt Bertha, and others) with computerized inventories of local medical and social service agencies. It is a standardized, web-based platform that is interoperable with medical and case management software.
Examples of resources include appointments at clinics, open beds at various shelters, food and clothing inventory of local relief organizations, spaces available in recovery/rehabilitation centers, and more.
-
The Community Resource eXchange will have a live referral function, which serves as a warm hand-off between providers at different agencies. Providers will know that when they connect clients to resources, the resources will be there.
Connecting patients to appropriate community resources helps them overcome social and economic determinants of health (i.e. stable housing, access to nutritious food, reliable behavioral health services, etc.). Supporting patients outside of the traditional medical domain helps solve the root cause of health issues, and ultimately leads to fewer costly and avoidable Emergency Room visits and Hospital admissions.
-
On their own, social service agencies have limited resources (staff, shelter beds, case managers, meals, etc.), and as a result case managers often refer clients out to other agencies to fill service gaps.
The Community Resource eXchange is designed to improve the efficiency and success of such referrals – through its live inventory function, care providers know that when they refer a client to seek resources at external agencies, the resources will be there. This function is interoperable with the shared care plans and allows providers to follow-up if clients are unable to obtain help through the referral.
-
Through its live inventory function, the Community Resource eXchange solves the issue of patients going somewhere only to find that the resource is no longer available. Patients will receive the right resources at the right time to appropriately address social and clinical barriers to health.
-
Over time, as we track which resources are in highest demand, we will be able to shine light on community-specific needs.
Community Care Coordination - Facilitates cross-agency care coordination
Our Community Care Coordination is a scalable model to provide compassionate care coordination across medical and social domains for our partners' most vulnerable patients.
Care coordinators and case managers at partner agencies bring the model to life by using our comprehensive, shared, web-based health record system.
Our comprehensive health record system stores records of all patient visits to participating agencies, telling a complete story of where a patient has been and why. Access to the record is dependent on a viewer‘s role and HIPAA designation.
Our Community Care Coordination model facilitates patient-centered care by structuring care plans around patients’ values and goals.
The technology that drives our Community Care Coordination model is unique in that it has a Referral Portal, which enables participating medical, social and government agencies to refer clients to one another to bridge the resource gap in real time.
Core functionalities enable our care coordinators to engage in secure, protected online discussion with providers from different systems who can shed light on the interrelated needs of clients.
As it is currently being used, the Referral Portal bolsters accountability by facilitating communication across provider systems, filling the need for a unified platform that enables efficient and timely coordination across agencies.
The software has been designed to continually record and analyze key data points around social determinants of health, which will ultimately inform policy on a local, state and federal level.
-
Not only will providers be able to see at which other agencies their patients receive services, but they will be able to read patient’s goals and values before meeting with patients. When providers know what is important to their clients, they can use goal-negotiated care models to achieve greater patient compliance and buy-in, and ultimately better health outcomes.
Our pilot program, in which our in-house care coordinators used our comprehensive health record system to document and measure patient outcomes, demonstrated measurable impact: It resulted in 41% reduction in hospital visits, 15% improvement in patient quality of life measures (DLA-20), and $15 Million in cost avoidance. This model, when scaled, promises to significantly improve the health safety net for Harris County’s most vulnerable patients, while saving the system millions of dollars.
To magnify the impact of this program in the community, our plan is to scale internal care coordinators to serve 300 clients/year, plus facilitate care coordination for an additional 1,500 clients through community partnerships in the next three to five years.
-
Our comprehensive case management software has been designed with both social service and medical agencies in mind to deliver the best care possible to clients with complex social, medical and behavioral health needs. The software enables case managers from different agencies to collaborate and see how clients have progressed in behavioral and health goals.
-
The Community Care Coordination model shifts patient care from a model centered around solving problems to a model centered first and foremost around patient values to increase engagement and patient satisfaction across the continuum of care. Additionally, through interagency case management, patients have an advocate to help them navigate a confusing, overly complicated health system.
-
As we gather further evidence about which social and economic barriers to health affect our community the most, we will have grounds to advocate for policies and legal systems that support more equitable access to health and well-being.
Who Benefits
Patients and communities are the ultimate benefactors of our Platform; in serving them we’ve quantified impact and savings for:
Case Studies
Lone Star Justice Alliance, Dallas County, TX and Williamson County, TX
Problem
Current criminal justice reform practices for youth populations have shown to be ineffective. Data clearly points out that criminal justice reform indoctrinates vulnerable youths to a life of regular involvement with the legal system. In our current system, there is an emphasis placed on punishment rather than reform. As a result, the rate of recidivism regularly exceeds 75%. Furthermore, 17-24 year-olds only comprise 11% of Texas’ population, yet they account for over 29% of state-wide incarcerations. Their probation is revoked three-times more frequently than older adults. Moreover, people of color within this age range are arrested at nine-times the frequency of their Caucasian counterparts. It is evident from these statistics that the existing system perpetuates an already high incarceration rate for young adults that will likely carry over throughout their later adult life—perhaps multiple times over for people of color.
Lone Star Justice Alliance (LSJA) is a nonprofit legal organization dedicated to improving the lives of these youths and emerging adults (17-24 years old) in the justice system through (1) the utilization of developmentally appropriate responses to behavior, (2) treating youth and emerging adults with equity and dignity to promote resilience, (3) conservation of costs, and (4) increased public safety practices.
Solution
A customized version of PCIC’s CIE has been designed to bring together the LSJA’s team, the court systems, district attorney’s offices and community organizations to (1) support an intervention for young adults through a values-based approach, referred to as an individual’s “spark” and (2) accommodate other needs of the care model specific to this project. Their care team, judges, and community partners can closely track progress and outcomes, determine resource availability and needs, make referrals, manage the intervention workflow and analyze data in one consolidated platform. Research partners of this project include the University of Texas Health School of Public Health, Texas A&M Public Policy Research Institute, and Harvard Law School’s Access to Justice Lab. The academic institutions are involved to design and conduct a randomized control trial (RCT) in order to track participants’ health and criminal justice outcomes. By pioneering this study, the collaboration aims to establish a new standard of transformative justice, health and social practices that are driven by data and evidence-based outcomes-- specifically health and criminal justice outcomes, perform cost-benefit-analysis, and process evaluations in the Transformative Justice Program. Results from the RCT will be disseminated to stakeholders in these counties and to researchers and experts at local, state, and national conferences in order to inform changes in policy that could reduce the state’s incarceration rate, while promoting public safety and the effective use of the state’s limited resources. This is the first study of its kind in the United States since the mid-1960’s, and it has the potential to provide the most comprehensive evidence in favor of treatment over incarceration.
To learn more about this project, visit the LSLA website at https://www.lonestarjusticealliance.org/
Houston Food Bank, Houston, TX
Problem
The Houston Food Bank (HFB) is Houston’s central agency for serving the city’s food-insecure population. Beyond this core function of distributing food to those in need of it, they have also created the Community Assistance Program (CAP), which helps individuals apply for state-funded social and health services, such as SNAP, TANF and Medicaid/CHIP, as well as linkage and referral services to other social service providers and other food bank programs. The program sends and receives referrals from a variety of agencies, such as HFB’s partners, public access systems and entities connected to their FIRST Link (Food Insecurity Resources Screenings Training) program, which ensures that healthcare partners around the city are cognizant of HFB’s services, by training clinicians and following up with patients to see if the referred resources have been given to them. Implementing this approach would provide tremendous assistance, particularly to the food-insecure and those in need of social services. In theory a network is established between HFB and agencies within their referral-base, which allows for an “no wrong door” approach to care provision. This means that an individual can go to HFB with any social or medical need, and if HBF cannot provide the service or treatment themselves, they will work with Community Resource Navigators (CRNs) from HFB’s Referral Partner Program (RPP) to identify and submit a referral to any agency within their network capable of meeting their needs. However, the steps required to achieve this are spattered with challenges. Currently, these additional services are tracked in separate disparate systems without the use of a unified solution. The complex workflows for both receiving and sending referrals from HFB without a dedicated solution to support robust electronic bi-directional linkage of services in the community limits the impact of this program. Given the expansion of HFB’s services, it also makes the tracking of outcomes across all Food Bank programs and at a broader community level much harder.
Solution
PCIC has rolled out the Community Data eXchange (CDX) module for HFB to integrate data from different Food Bank data systems, spanning the greater Houston area, to gauge how combatting food insecurity can have a positive cascading effect on the social, economic, and health outcomes for individuals utilizing the Houston Food Bank’s resources. This data sharing and processing will inform and direct HFB’s RPP coordinators to the optimal referral agency to meet a patient’s unique set of needs.
In addition to the CDX, PCIC has rolled out the Community Resource eXchange (CRX) and Community Care Coordination (CCC) modules of the Unified Care Continuum Platform (UCCP) to manage and track activities within the CAP and FIRST Link programs. This provides a unified platform for tracking as well as real-time, bi-directional, electronic referrals both within HFB, as well as to external community partner organizations. Additionally, the using the platform closes the communication loop between agencies, by integrating direct SMS text, voice calling and email features into the CCC interface. All these features culminate to provide HFB with tools to connect individuals to resources, internally or externally, in real-time, while keeping those within the loop informed of their medical and social service history. PCIC’s UCCP combined with the training on PCIC’s Values-Based Model of care creates a holistic approach – integrating data, a care model and resource connectivity that can be scaled to all Food Banks nationally.
To learn more about Houston Food Banks CAP program and other service, visit the Houston Food Bank website at www.houstonfoodbank.org
Partners in Primary Care, Houston, TX
Problem
Clinics systems like Partners in Primary Care (PIPC) provide essential services around primary care needs for patients and are starting to look at Social Determinants of Health in a new way, by bringing the service of connectivity and referrals to Community Based Organizations (CBOs) within the clinic setting. PIPC does this by having care coaches at the clinics, who fulfill the role of a care coordinator. This role involves engaging with a patient in a one-on-one setting to establish an individualized care plan, that includes coordinating resources and services outside of the PIPC clinic system, based on the needs and goals of the patient, and it can be accomplished by a variety of board-certified healthcare professionals, from doctors to physician’s assistants to resident nurses, etc. In doing this, care coaches are fostering an environment that proactively involves the patient in the treatment process, thus motivating them to take control over their own “health journey”, increasing retention rates and improving outcomes. However, while this is a holistic and innovative approach to health management, the infrastructure to accomplish these goals is lacking—there is no coordination between the agencies providing care to a given individual. The communication barrier between cross-sector agencies, on the patient and community level, and the lack of a central patient-tracking platform contribute to the siloed nature of care in the current healthcare system. The challenges are particularly acute for clinic systems, such as PIPC, that face bottlenecks in the referral process—for a high-traffic agency that provides and relegates care, efficiency and timeliness are key components that are missing to improve patient outcomes. This means that while someone may eventually receive the resource they need, the process is inefficient, and in periods of scarcity, the resource may not be available at the time of need. For care coaches, the inability to track the utilization patterns and health outcomes of receiving individuals and agencies participating in this process further complicates the ability to construct, analyze and follow through with a care plan. In order to overcome these challenges in the system, a comprehensive solution must be in place that integrates cross-sector data sharing, care planning and care coordination functionalities on unified platform, centered around an individual’s needs.
Solution
PCIC and Partner’s in Primary care (PIPC), a subsidiary of Humana Inc. dedicated to providing patient-centered care to those looking to overcome an ailment or simply maintain their health, have launched an initiative to connect community-based resources to PIPC’s members that are in need of social services, such as food insecurity, economic instability, housing, etc. PCIC’s Community Care Coordination (CCC) and Community Resource eXchange (CRX) platforms will provide PIPC’s care teams a way to coordinate social and medical services, through real-time referral integration, manage individual care plans, share HIPPA protected patient health information (PHI) and track members’ abilities to address Social Determinants of Health (SDoH) needs, while providing an excellent member experience and increasing retention rates among PIPC’s Houston-based members. The Community Data eXchange will serve as a data reservoir, from which PCIC’s team of data analysts can determine geographic resource mapping and utilization patterns around the city. These functions are supplemented by PCIC’s training on the Values-Based Model approach to care to allow PIPC’s care team to efficiently construct an individualized care plan for each member.
Legacy Community Health, Houston, TX
Problem
Legacy Community Health (LCH) has integrated a patient-centered model of care for all individuals within their system—a model that promotes wellness beyond medical aid and has the potential to provide a structure that promotes independent and sustainable health practices. Furthermore, they have made it part of their mission to coordinate social services, along with the clinical services they already provide, to their high-needs, high-cost patients (HNHC). Their efforts begin by determining the patient cohorts within their system that would need such services, then, a team of Health Advocate Student Interns (HASI) schedule one-on-one appointments to construct a care plan around their specific needs and obstacles. However, the path to achieving this is littered with siloes, open communication loops and a lack of communication between the sectors of care. For example, systems, such as Electronic Health Records (EHRs), previously LCH’s only viable system for identifying patient health information, may be able to convey the basic health status and medical history of a patient, but without an integrated referral function, the platform has limited use cases. Furthermore, the existing EHRs are void of Social Determinants of Health (SDoH) tracking features, thereby excluding a major aspect of a comprehensive health management plan. Without a central platform on which SDoH-integrated care plans can be constructed, resources coordinated, outcomes tracked and participating agencies can view and comment on patient profiles in real-time, the capacity for a sustainable care coordination model is out of reach.
Solution
PCIC is providing support to LCH by creating a bespoke version of the Community Resource eXchange (CRX) and Community Care Coordination (CCC) modules. Additionally, PCIC is working with the data provided by LCH to develop a tool capable of screening for Social Determinants of Health (SDoH) and providing an overlap analysis of agencies that are frequented by their patients. In doing so, LCH care team members will be able to identify the individuals that fit the HNHC criteria and map resource utilization patterns. Thus, a cohort of preferred agencies are identified and focused resource mapping is achieved to optimize and streamline the referral process. By doing this, LCH’s team of HASI can use the screening tool to determine individuals that fit the HNHC profile, based on a pre-determined set of inclusion and exclusion criteria. On a daily basis, LCH’s patient data will sync to the CCC and CRX to ensure that information is always up to date. This is especially useful for scheduled appointments, as the screening tools and Protected Health Information (PHI) for each patient is prepped and ready upon the patient's arrival. Furthermore, the cloud-based interface of the CCC along with the referral functionality of the CRX will be used to combat the siloes that previously prevented a smooth and comprehensive care coordination flow. Using this system means that LCH will have a method of linking referrals, not only to other clinics and hospital systems, but also to social service agencies and Community-Based Organizations.
Integrating outcomes assessments, real-time, two-way communication features with all participating agencies (emailing, phone-calling and text messaging) and care plan management tools into the platform means that the HASI team will be equipped with the tools to seamlessly and efficiently provide care coordination services to their HNHC patients, while closing the loop on cross-sector communication and PHI sharing. Critically, this model has the potential to scale across the national healthcare system and manifest a new norm of improved outcomes for patients, real-time referral management and a reduced cost to the system.
To learn more about Legacy Community Health’s work, visit their website at https://www.legacycommunityhealth.org/
Harris Health System, Houston, TX
Problem
The Harris Health System (HHS) is the largest health system in the nation’s third most populous county, Harris County, and it contains a wealth of data representing Houstonians. In the recent past, the sharing and application of such information, from PHI to resource utilization patterns to metrics regarding the engagement of patients with agencies within HHS has been limited in use. For example, if a patient within HHS initially receives care from Ben Taub General Hospital (BTGH), their renown Level 1 trauma center, then later goes to Lyndon B. Johnson Hospital, HHS’ largest acute care center, the only information that is tracked between the two entities is the PHI, thereby inadvertently neglecting the bigger picture—the need to find a comprehensive solution to the patient’s health story rather than just addressing temporary, immediate needs. Furthermore, with the understanding that each patient has a different level of need, HHS has no way of stratifying patients in their system based on their needs and offering supplementary services to those who fit the description of a high-needs, high-cost individual (HNHC). Using data to understand the who, what, when, where, why and how of HNHC individuals’ would allow HHS to target specific patient demographics (in terms of condition and geography) for additional care, mobilize resources to entities within the system according to their capacity form strategic partnerships to meet logistic and care-based needs identified. The existing lack of intra-system communication has perpetuated the siloed nature of care prevalent in health systems across the country. Without a meaningful use for these data, it is difficult to improve upon the existing system in terms of providing individualized care, improving health outcomes for patients and reducing the cost of care per capita.
Solution
Since 2015, PCIC has incrementally increased involvement with HHS’s population health team to facilitate a regular data “dump” schedule to the Community Data eXchange (CDX), in which data from HHS can be analyzed to answer the following questions: Which patients within the system are considered High-Needs, High-Cost (HNHC)? What are the specific needs for certain patient cohorts—how can the path to delivering such treatments be expedited? On what frequency basis do certain patient cohorts visit ERs (or any other type of agency) within the system? What are the reasons behind visiting the ER for those who frequent it? By addressing these questions, the holes in the current care model can be identified and remedied to overcome the issues previously present— generalized (and sometimes ineffective) care, stagnant community health outcomes and exorbitant cost per patient. Since the beginning of the partnership in 2015, the width of data transferred, in terms of the type of demographic information conveyed, has expanded greatly, giving PCIC’s data analysts the ability to construct highly specific data dashboards that visualize resource maps around the city, maps to identify areas particular affected negatively by Social Determinants of Health (SDoH) and utilization patterns within the system, among other metrics for use by HHS. This increasing data load for an already expansive system demonstrates the scalability of such a platform to other health systems. HHS’ team of navigators, individuals tasked with coordinating supplementary services for patients, can use these dashboards to understand the imminent needs of patients in their system on an individual and community level, particularly for those who are frequent users of their main ERs, at LBJ and BTGH. Moreover, by working with PCIC to develop data-driven inclusion and exclusion criteria, HHS can now identify their cohort of HNHC patients, otherwise known as their “MVP” patients, and use the tools integrated into the Community Care Coordination (CCC) and Community Resource eXchange (CRX) modules to communicate with and refer their MVP patients to external agencies capable of providing care, in real-time. Additionally, PCIC’s intervention team has played a consulting role for HHS’s care navigators by providing assistance to enroll patients into the system, training care providers on the Values-Based Model of care, and advising on best practices for patient interaction.
Humana, Houston, TX
Problem
Public data and data from large health-solutions corporations, such as Humana, represent a massive, untapped resource for the healthcare industry. The more that is understood regarding the demographic distribution of people, their needs, the resources they use and the facilities they visit, the better the disparities and shortcomings of the healthcare system can be understood. Without this context, the efficacy of care provision cannot move past the individual level. To truly tackle holes in the system on a community-wide basis and coordinate care efficiently and effectively, a holistic understanding of the population of interest, in terms of their demographic information, geolocation, behavioral trends and patterns, must be established. The existing model of care across health systems nation-wide have perpetuated the status quo, by ignoring these data or failing to incorporate it constructively, with the intent of increasing efficiency, improving the patient experience and patient outcomes, and reducing the physical and monetary cost to the system.
Solution
PCIC and Humana have partnered to create a bi-directional data feedback loop on the Community Data eXchange (CDX) module. What this means is that data from Humana’s expansive database along with a plethora of public data (e.g. from the census, CDC, etc.) are transferred to the CDX for further cleaning and manipulating to identify holes in the system. By accumulating data from such a variety of sources, PCIC’s data team can represent, with great precision, community-wide metrics regarding population health parameters. For example, PCIC has developed dashboards to visualize resource utilization patterns, hot-spot maps, depicting the density of food-insecure people across the city and overlap maps, showing which agencies are most frequently used by this population. By providing Humana with these analyses of their data, a closed feedback loop is established that conveys specific areas of need and the agencies and resources available to support such a need. Thus, several intermediate steps are avoided in the care coordination/ care provision process, cutting down on the time and cost required to deliver quality, individualized care.
Unified Care Continuum Platform breaks down silos in care for clients of Recovery and Rehabilitation Center
Problem
The Houston Recovery Center partnered with PCIC to address a lack of data sharing in the community. The Center noticed a very silo-based model of case management in the Houston area: Although they knew that their clients were interacting with a broad array of social and medical service agencies across the city, none of the agencies could see what care their clients were receiving outside of their own walls. This resulted in inefficient case management, and many missed opportunities to communicate and collaborate across agencies.
Solution
PCIC linked HRC’s patient visit data with over 8 million patient visit records that exist in our Community Data eXchange (through existing partnerships with other social and medical agencies). To make this data meaningful to HRC, we built a customized, de-identified (HIPAA protected) dashboard for HRC that shows which other provider systems their patients frequent, how often they frequent them, and what services they receive there. This aggregated all the providers and services that their patients were utilizing into a single, global perspective.

We serve complex, high cost clients. PCIC confirmed it. Now we clearly see the community providers that also serve our clients. The usage patterns and costs are staggering.
PCIC provides a platform to develop systems of care coordination to improve health outcomes. This opens a brand-new door to preserve community resources and manage population health.
Program Manager - Houston Recovery Center
Copyright © 2025
Patient Care Intervention Center. All rights reserved.
Team Site