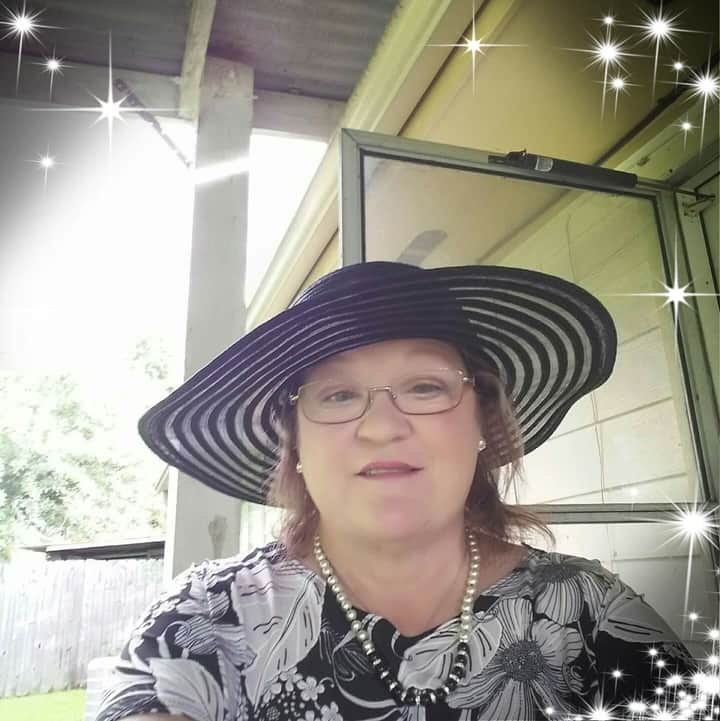
Ms. Stephanie
Finding HomeFor Ms. Stephanie, complications from Chronic Pulmonary Disease, Peripheral Vascular Disease, and an amputation to her right leg, caused by mismanaged Diabetes, limited her independence. On top of the physical limitations these chronic issues caused, she was struggling to maintain a positive outlook and was unable to maintain a state of mental well-being.
Dawn Washington, one of PCIC’s experienced MSWs, worked with Ms. Manners, both during and after the intervention period, to coordinate services that would restore her independence. This began by connecting her to a Metrolift pass, to take the buses and trains to her medical appointments on her own accord. To ensure she was secure with meals and snacks during the day, while Stephanie’s daughter was at work, Dawn coordinated to have Meals on Wheels provide food for her daily. When she suffered an infection from her amputation site, Dawn also scheduled appointments with her specialist to have the issue addressed in a timely and efficient way, before any further complications manifested.
While these measures were taken to provide stability and comfort to Ms. Stephanie during a tumultuous and unfamiliar stage in her life, on top of the existing difficulties brought about by COVID-19, she knew that her ultimate goal was to move back to Louisiana, where her actual home is. With Dawn’s help, she had transitioned back to her house in Louisiana by the time she graduated PCIC’s care coordination program, where she currently has the assistance of an individual home health aid four days per week to help her manage day-to-day tasks. Additionally, her local church providing meal assistance and transportation to her medical appointments have been a tremendous help to her. Above all, however, Dawn provided a listening ear and willing hand to Ms. Stephanie when her situation seemed absolutely bleak.
Dawn has been like my family I can depend on with truth, integrity and knowledge. What she doesn't know—she doesn't keep me hanging. She always gets back to me. She is a blessing and answer to my prayers. The best of people that helps me […] She goes far beyond the call of duty. I absolutely love her
We are proud of Ms. Stephanie for her unwavering persistence despite an unrelenting combination of difficulties coming her way, and we are thrilled that we could help her attain her ultimate goal safely and in better health than she was before!
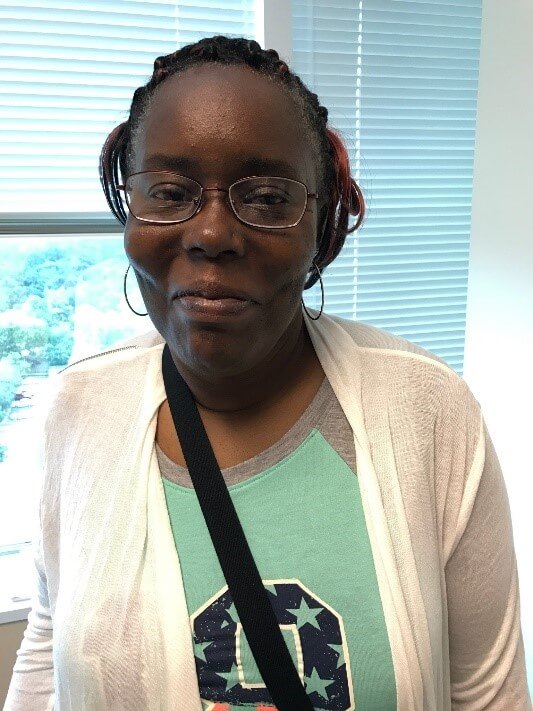
Mrs. Thelma
Keeping FaithGoing to the doctor should not culminate in backwards progress. Unfortunately for Mrs. Thelma, the last few years of hospital visits have resulted in just that. Suffering from diabetes and severely painful intestinal and urinary complications, including chronic constipation, motility issues, and mishandled UTIs, among other ailments, she was a frequent user of emergency medical services that brought her little to no lasting relief.
She points out that one of her biggest barriers to achieving a more sustainable, healthy life is a lack of effective communication with her primary care physician (PCP). Her appointments entailed seeing a variety of different nurses and residents, none having the full context of her medical history. Moreover, she felt the myriad of clinicians discounted her self-evaluation, largely due to her age. This miscommunication resulted in a persistent cycle of going to the doctor to receive prescriptions for medications that caused painful side-effects, which led to another hospital visit. She simply wanted to consult with her PCP and have her voice heard. After enduring 19 surgeries and many years of unresolved pain, she was losing faith in a medical field that conditioned her to expect no real change. Her story is the reality that exists for many complex patients even if they are covered by Medicare or Medicaid.
Currently, PCIC’s Tara Pitts, MSW, is attending doctor’s appointments with Mrs. Thelma to ensure that her PCP is attentive to her values and needs, as opposed to sending an ever-changing group of trainees to tend to her. By serving as a liaison between Mrs. Thelma and her PCP, Tara‘s experience in the field helps clearly articulate Mrs. Thelma’s concerns, and ensures that the appropriate actions are followed to make lasting changes in her health plan. In Mrs. Thelma’s words, PCIC has given her the “mouthpiece” to gain the respect and attention she deserves when interacting with her PCP.
Although Mrs. Thelma has been in great pain, she still finds ways to be a light in her community by participating in her church’s choir (as a tenor), and volunteering at several food drives and nursing homes with the help of her tremendously supportive husband, Mr. James. In his words, “she is not meant to be house-bound”. We couldn’t agree more. She is still on the path to recovery, but for the first time in a long time, it’s finally in the forward direction.
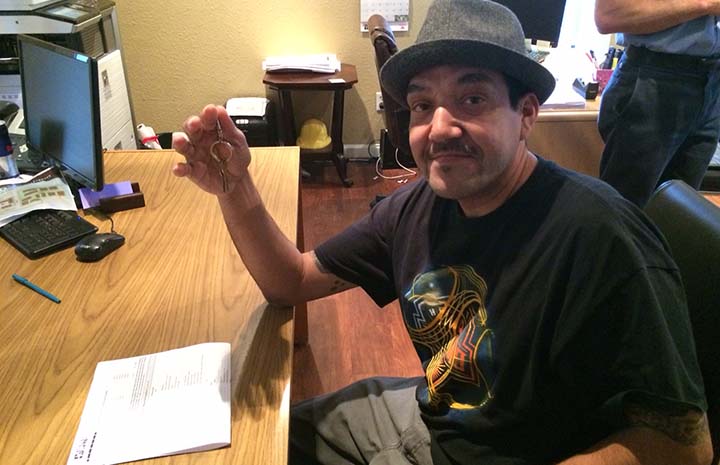
Mr. Garry
The Power of Personal TransformationIf you had met Mr. Garry a year ago, you would have found him homebound living in his sister’s living room, with foot problems due to diabetes, and very isolated. He relies on public transportation, however, he lived two miles away from the nearest bus stop and it was too painful to walk there, so he was stuck.
His insurance provider referred him to PCIC for care coordination services after he visited the emergency room 24 times in one year. He was not admitted to the hospital on any of these visits, which indicated that his problems could have been better addressed in a clinic.
Very quickly our care coordinators established that Mr. Garry's medical needs were only a fraction of the problem. They began accompanying him to his medical visits, enrolled him with a Medicaid transport service, and helped him and his sister move to a place where he could have his own bedroom.
Now that he is receiving regular treatment for his feet, he regularly walks by himself to the grocery store, Medicaid Transport helps him get to and from his medical appointments and even takes him into a local community center where he volunteers once a week.
When our care coordinators presented Mr. Garry with his diploma, his sister reflected on the progress he had made in just six months. She said, “I can’t believe they care about their patients so much that they’d offer services like this. I’ve worked in home health for a long time and not once have I experienced something like this.”
Ms. Maggie
Taking the driver seat on the path to independenceBefore Ms. Maggie joined PCIC's intervention program last fall, she was struggling to find affordable transportation to and from her many doctor appointments and the pharmacy.
Determined to make all of her key medical appointments, she was paying out of pocket for Lyfts and Ubers and was left without enough money for basic needs. Additionally, due to this transportation barrier, she had not been able to see her primary care provider for over four years, since the office was far away.
As a new graduate of PCIC’s intervention, Ms. Maggie feels more hopeful towards her health.
She is now connected to reliable Medicaid transport, visits her new primary care physician regularly, and independently schedules and attends all of her own medical appointments.
Perhaps most significantly, after waiting for eight months, she finally received a much-needed heart surgery.
In her own words, Ms. Maggie shared that she was grateful to PCIC's Victoria Bryant, MSW, for supporting her when she lost her father. Ms. Maggie's niece and great-nephew were present at her graduation.
Ms. Debra
"Just to get better, get surgery, and move on...I want to be there for when my grandchild is born"Twenty years is an extremely long time to live with a treatable illness. Unfortunately, the pain and suffering was the only option Ms. Debra had as she was the primary breadwinner and care-taker for herself, her mother, and her adult son who is disabled and legally blind.
As a teen, Ms. Debra was one of the first patients to receive a minimally invasive weight loss surgery. However, over a period of twenty years, she developed significant esophageal scar tissue as the band migrated from her upper stomach to her esophagus. For fifteen years, she felt discomfort and occasionally had trouble eating, but she was not financially able to take time off from work to seek treatment.
Ms. Debra's condition became so severe in the past five years that the scar tissue is preventing her from eating anything except liquids. It is causing her to be undernourished to the point of needing emergency care. In addition, she faces great systemic barriers to healthcare: lack of health insurance, lack of transportation, and limited hospital and outpatient services in her rural neighborhood. These barriers delay necessary treatment and surgery and all Ms. Debra wants is, "Just to get better, get surgery, and move on...I want to be there for when my grandchild is born."
Currently, PCIC is working together with her private and county providers to help Ms. Debra attain necessary surgery and integrate her care efforts across health and social service agencies. We are also in the process of securing home health services to relieve Ms. Debra from her significant care-taker responsibilities. Our work helps patients like her secure critical outpatient care, reliable transportation, and social services, ultimately preventing further health deterioration.
Ms. Charlott
One step closer to better health. Thanks to PCIC!Ms. Charlott, a woman well known to nurture her loved ones and neighbors, suffers from chronic abdominal pain. The pain combined with daily stressors is assumed to cause the seizures she also suffers from, and the severity of her abdominal pain keeps her in bed – the last place a natural caretaker and social butterfly longs to be.
She would frequent the Emergency Room to reduce her crippling pain, but she went with very little confidence that she would find a way to cope. Her five different specialists couldn't provide a solid diagnosis for her illness or her seizures because of vague symptoms, an unconfident patient, and too little time during visits to sort through several different sources of data. Communication between Ms. Charlott and her providers was lacking, and the lack of communication between her multiple providers were causing the situation to become worse.
Unfortunately, our health system is ill equipped to communicate across specialties and recruit vital social resources for patients. Luckily, PCIC is working with patients like Ms. Charlott to create realistic goals as well as design communication pathways with hospitals, providers and social service agencies to inform each other of each High-Need, High-Cost individual’s care plan. For Ms. Charlott, we targeted her goals (fewer debilitating days from her pain and seizures), provided resources based on her goals (durable medical equipment like a wheelchair), and we also coordinated appointments between her many specialists to get her closer to her desired health outcome – less pain and less seizures so she can finally return to taking care of her friends and family.
Mr. Trondail
PCIC helping build his support systemMr. Trondail is an ambitious man who hopes to reunite with his son and return to school to finish his degree, but he is also homeless and suffers from a chronic condition he has neglected for years. Like many High-Need, High-Cost patients he had a difficult time managing his health because his values continued to be overlooked. The one aspect of his life, other than his son, that he values most– his dog Striphe (pronounced Stripe) – continued to be a missed opportunity in a medicalized approach to health.
With 12 Emergency Room visits and 2 hospitalizations under his belt in the span of year, Mr. Trondail continued to have poor outcomes that were continuously exacerbated by systemic barriers – he was not able to get housing, a job, or regularly access expensive medicines he desperately needed.
At PCIC we are focusing on using patient-centered care to take notice of psychosocial factors that are largely overlooked: patient values, systemic and individual barriers, and nonmedical approaches for measurable outcomes. With Mr. Trondail, changing healthcare tactics to address the root cause of his medical and social barriers, allowed our Care Coordination Team to enroll Striphe as an Emotional Service Animal, connect Mr. Trondail to appropriate physical and mental health resources, and successfully place Mr. Trondail and Striphe into an apartment of their own.
Ms. Loretha
Dreams have become realityAn extreme utilizer of Emergency Medical Services (EMS) calls and transports, Ms. Loretha felt powerless managing her health. Struggling to manage COPD, anxiety, depression, and chronic headaches, she felt trapped - afraid to go outside for fear of exacerbating her COPD.
Fortunately, we identified her through fire department data as a High-Need, High-Cost patient, and intervened - coordinating health and social care, providing advocacy, building trust, and linking her to a provider.
When our team first started working with her, she could not walk the length of her driveway without becoming short of breath, but she successfully graduated accomplishing six months of our Intensive Care Management program, and is proud to say she can now coordinate her own care.
Dreams becoming reality, Ms. Loretha can run around outside with her grandchildren without becoming short of breath.
Ms. Cynthia
Successfully completed our program for a better tomorrowHungry. Homeless. Ms. Cynthia, a diabetic and former drug addict, struggled with high blood pressure and lupus. She frequently called 911 when she didn't feel well. Missed doctor appointments were the norm due to her transportation challenges. Then a disengaged partner became detrimental. Realizing she'd hit rock bottom, she was open to help. PCIC reached out by setting up dependable transportation to help her keep appointments. Services were set up for a glucometer and lancets. Training to log blood glucose levels was provided. A PCP and other specialists were also arranged. She has continued to lean on us for support when she reverts to unhealthy patterns.
Ms. Cecelia
PCIC didn't give up, so why should sheAfter the death of her mother, Ms. Cecelia lost her life-long companion and primary care-taker. Unable to live independently, her living conditions and medical care took a sharp decline. Constant falls and HFD transports related to unmanaged diabetes and congestive heart failure made it difficult for Ms. Cecelia and her family to cope.
After PCIC's intervention, Ms. Cecelia transitioned to a supportive nursing facility and got connected with specialty physicians focused on stabilizing her conditions. She has had a 81% reduction in ER visits and hospital admissions.
Mr. Lee
Saving livesUntil early 2000, Mr. Lee worked as a surveyor in Texas and enjoyed the outdoors. However, he caught our attention as a likely High-Need, High-Cost candidate in early 2015 because of his repeated 911 calls. When we reached out to him, we found him wheelchair-bound, enslaved to alcohol, severely undernourished and alone. He had become a High-Need, High-Cost patient mainly because of his chronic pain. Despite his enrollment he remained reclusive and uncooperative until one fateful day in April, when we found him at the end of one of his severe drinking binges.
He was lying in bed, soiled and hungry from going days without eating. He said he wanted to end his life. His blood alcohol level was five times the legal limit. Mr. Lee was admitted for medical detox on the same day, followed by psychiatric care one week later. With the assistance of the Mobile Crisis Outreach Team and "A Place for Mom" we were able to coordinate with both Mr. Lee and his brother in finding an assisted living facility. Mr. Lee now benefits from regular meals, appropriately dispensed medications as well as a Primary Care Physician who oversees his chronic medical problems. Until PCIC came into Mr. Lee's life, his family had thought he was a 'lost cause' since he had given up on himself. With the help of our team, his health continues to improve and he's able to manage his pain and alcohol dependency. His family once again is taking an active part in his life and he no longer needs to call 911 for medical care.
Mr. Jesse
Thank you for always showing upSleeping on a bench outside his family home, Mr. Jesse constantly cycled in and out of the ER as his blood sugars alternatively spiked and plummeted. Without consistent access to food or insulin, he struggled to manage a particularly treatment-resistant case of type 2 diabetes. Years of struggling with unmanaged diabetes and homelessness had left him in chronic pain and without hope.
PCIC and Mr. Jesse worked together to find a new home and connect him with the medical and social services he needed. Since PCIC's intervention, Mr. Jesse is stably housed and well-supported with a 50% reduction in ER visits and hospital admissions.
Mr. Randy
PCIC intervention helping improve quality of lifeRandy worked on an oil rig, and after enduring a traumatic injury on the job, his life became challenging as he lost his job, his family, and his home. Feeling discouraged, he became an alcoholic and enrolled in rehabilitation programs; but that did not help him address the unknown causes for his seizures. Because he was homeless, 911 was usually called by a bystander who witnessed the seizures.
Having attended several programs that failed him, he was surprised and pleased to see that PCIC was consistent and passionate about helping him. Through care coordination we connected him with a primary care physician, decreased his ER visits, and he hasn’t had a seizure since enrolling.
During this time he’s also managed to develop a healthier relationship with his son, who is his motivation to get his health and addictions under control. He has been very compliant and cooperative throughout the entire process, and has maintained a very positive attitude towards improving his health.
Mr. Travis
It may be stormy now, but it never rains foreverSuffering from priapism and high blood pressure, Mr. Travis, a timid and shy man felt hopeless and depressed. This childhood disease revealed in adulthood made him fear for his life. A needed change in diet spurred his well-intending mother to cook foods that exacerbated his condition.
When asked what he should do when he had flare ups, a health professional directed him to "just call 911", and prescribed him counter-productive medications. PCIC intervened to coordinate his care. We found him a new doctor, helped guide dietary and lifestyle changes, and nourished his will to live. A new confidence and motivation enabled him to self-advocate resulting in a 75% reduction of ER calls, and most importantly, he was now in control of his life.
PCIC intervention helping improve quality of life