The Multiplier Effect
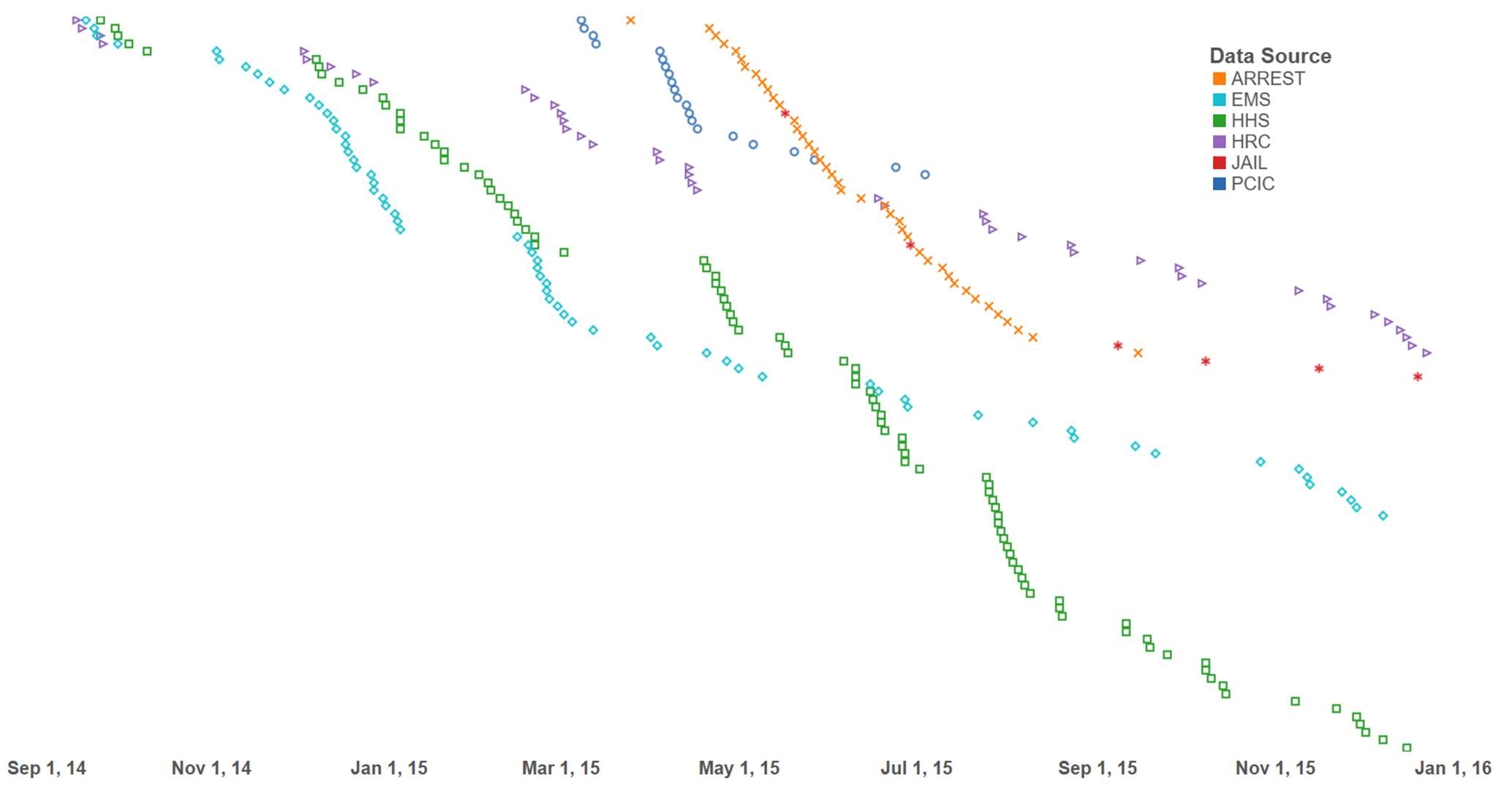
At PCIC, we work with the most vulnerable and marginalized patients, but also the most costly to the system. One of our clients – Client J – offers a striking example. Mr. J is a 59 year old male who started drinking when he was 18 and hasn't stopped for 41 years. In a little over a year, Mr. J had been transported by the EMS system 65 times, arrested 76 times, and been to the public hospital system 95 times, in addition to an astounding 44 visits to the Houston Recovery Center and 6 bouts in jail. Chart below shows Mr. J's overlap:
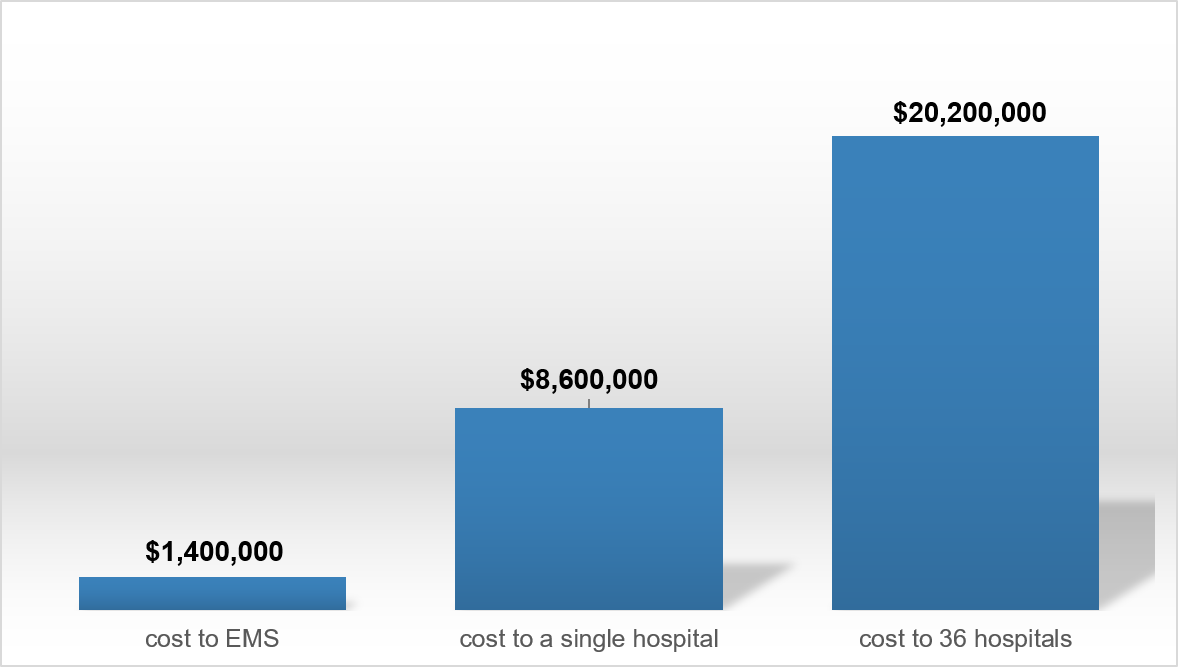
Using Harris Health System (HHS) data, the Houston Fire Department (EMS) data, and PCIC intervention data for one year, we identified the top users of EMS and projected their costs to a single hospital as well as to the entire network of hospitals in our county.
The top 1% of users of EMS (also the top 5% of High-Need, High-Cost patients at HHS) – 53 patients – were transported to 36 different hospitals in 12months, costing EMS $1.4 million.
To the public hospital system, they cost HHS $8.6 million in one year. Projecting the costs to the rest of the hospitals they were transported to, the cost estimates upwards of $20 million.
These patients make it clear that we can no longer view the system through silos. While the burden a single hospital bears is high, it does not compare to the multiplicative impact all the hospital systems experience.
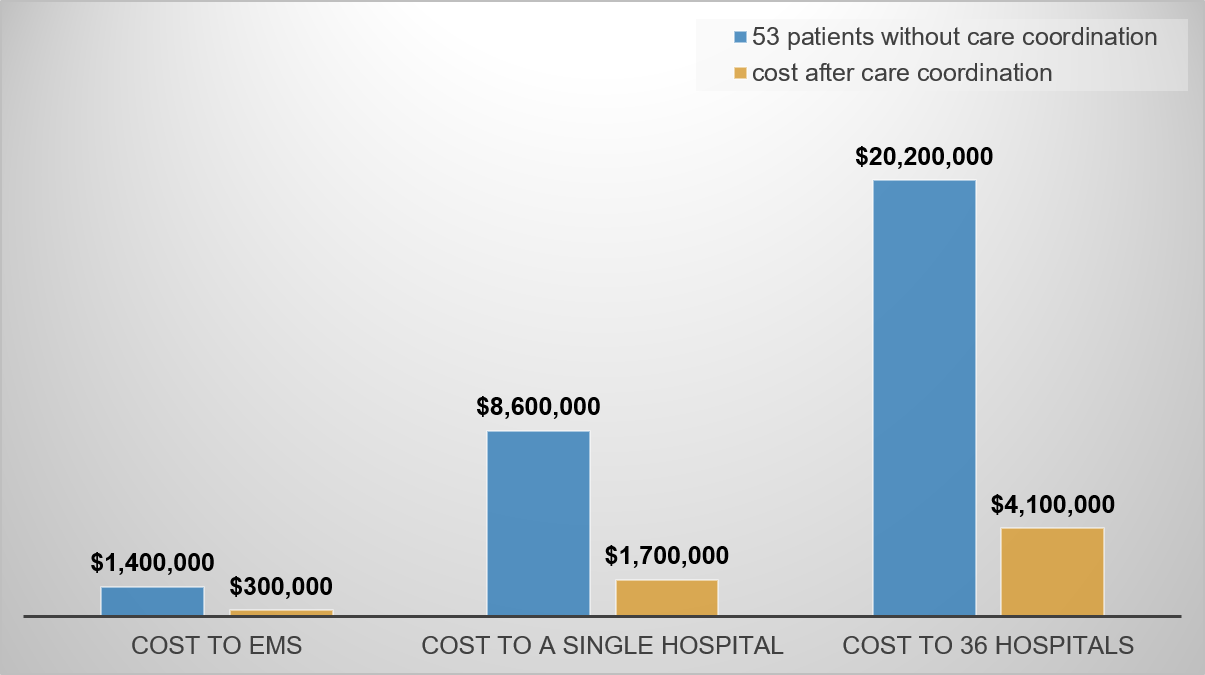
Through care coordination enabled by community-wide data sharing and cross-system collaboration, we can achieve immense gains in cost savings as quality of life for our patients by minimizing fragmentation.
If the above 53 patients were enrolled in the PCIC intervention, we project the cross-system care coordination would save the collective of the above 36 hospitals upward of $16M dollars (assuming 80% reduction shown in PCIC pilot).